Introduction
Knee osteoarthritis (KOA) is one of the most common chronic degenerative joint diseases, characterized by pain and dysfunction of the affected joint. Globally, the population of patients with KOA increased in the past 20 years, up to 2019, more than 350 million patients have been affected by KOA,1 leading to a great burden on health system. China has a large population of KOA, according to Global Burden of Disease (GBD) 2019, the incidence of KOA increased by 128.7% in 2019 compared with 1990, which was 84.258/100,000.2 Moreover, several studies have demonstrated that the prevalence of KOA in rural areas of China was significantly higher than that in urban regions (16.9% vs 11.1% in one study).3,4 The different prevalence could be associated with the different lifestyles (more manual labor in rural areas) and medical systems (low level of healthcare in rural areas). Therefore, we need to pay more attention to patients with KOA in rural areas.
Pain and dysfunction disturb mostly patients with KOA, and non-steroidal anti-inflammatory drugs (NSAIDs) are the most common prescription for KOA to relieve pain;5 however, NSAIDs cause adverse events in gastrointestinal and cardiovascular systems, which limits the usage among patients with KOA.6 Non-pharmacological treatments include education, weight loss, and exercise. The structured program of diet and exercise helps patients lose weight (for those who are overweight) and strengthen lower extremity muscles. However, inappropriate exercise may exacerbate the knee and increase the burden on elderly patients; therefore, a professional physical therapist is necessary for producing a personal program.7 Other treatments such as knee arthroscopy and knee replacement are suitable for patients with severe clinical manifestations, and they are costly, which might not be first chosen for patients who live in rural areas.5
Acupuncture has been widely used and studied as an alternative therapy for KOA in clinical practice, a study has demonstrated that three sessions per week of manual acupuncture for KOA were effective and safe.8 Another study has suggested that compared with sham acupuncture, intensive electroacupuncture had a better effect in relieving pain and improving function among patients with KOA.9 However, the selected acupuncture points in these two studies were all located in the local regions around the knee. According to the meridian theory, certain distal points are effective for KOA, LI11 (Quchi) is one of the points. Moreover, studies have indicated that certain regions of upper limbs and lower limbs are derived from the same primitive body segment, which still has an association with the development of human body.10 Also, several studies have confirmed the effect of LI11 in treating KOA.11 Therefore, LI11 is an ideal selection for acupuncturists working in community hospitals in rural areas or young acupuncturists due to the effectiveness, safety, and convenience, as well as for patients with KOA in rural areas due to the minimal invasion and low cost.
However, there is no study comparing the effect of LI11 and local acupuncture points for patients with KOA; thus, we aimed to conduct a pilot randomized controlled trial (RCT) in rural areas of Beijing to detect the effect of LI11 for pain relief and function improvement in patients with KOA.
Methods
Study Design and Setting
Our multi-center, three-arm randomized controlled trial (RCT) was conducted according to the Declaration of Helsinki and was approved by the research ethic committee of Peking University Third Hospital Yanqing Hospital (No 202000102). The intervention included 4 weeks of manual acupuncture therapy and 4 weeks of follow-up. Our study was registered on Chinese Clinical Trial Registry (Registered number: ChiCTR2000034926). Our study followed the Consolidated Standards of Reporting Trials (CONSORT) reporting guideline.12
Participants
Participants were recruited from the outpatient units of acupuncture and moxibustion department at Peking University Third Hospital Yanqing Hospital and Nancaiyuan Community Hospital. The enrollment started in June 2020 and ended in May 2023.
Diagnosis Criteria
Our study used the “consensus of four-stepladder program of knee osteoarthritis (2018)” to diagnose KOA. Participants were diagnosed with KOA if they met the following first situation and any two of the second, third, fourth or fifth situations.
- Chronic knee pain for the last 1 month
- X-ray confirmation of narrowing of articular space, sclerosis and/or cystic degeneration of subchondral bone, and osteophyte formation at articular margin
- Age ≥50 years
- Morning stiffness ≤30 min
- Bone friction sound (sensation) on movement
Inclusion Criteria
- Aged 50-70 years, male or female
- Diagnosed with KOA based on the abovementioned diagnosis criteria
- X-ray confirmation of Kellgren-Lawrence grade I, II and III within 6 months13
- Agreed to refrain from the routine use of analgesics; If participants needed rescue medication, they were provided ibuprofen (SK&F Co, Ltd, Tianjin, China; 0.4 g/8 hours).
- Written informed consent
Exclusion Criteria
- Had knee surgery or waiting for surgery
- Knee pain caused by other diseases (eg, tumor, autoimmune disease, trauma, and infection)
- Had arthroscopy within 1 year or intra-articular injection within 4 months
- Had acupuncture therapy within 3 months
- Had serious acute or chronic organic or mental disorders
- Pregnant or breastfeeding women
- Coagulation diseases (such as hemophilia)
- Had participated in other clinical trials within 3 months
Randomization and Allocation Concealment
Eligible participants were randomly allocated to the local point group (Control Group), LI11 (Quchi) group (Treatment Group A), or a combination of local point and LI11 point group (Treatment Group B) in a ratio of 1:1:1. The randomization sequence was generated with the R software (4.2.1), and we used minimization to minimize the total imbalance between treatments over multiple baseline covariates. We defined age, Body Mass Index (BMI), Kellgren-Lawrence grade, and center as baseline covariates with weight of 1, 2, 3, 1, respectively, and the allocation probability of Control, Treatment Group A, and Treatment Group B was 0.6, 0.3, 0.1. All processes were done by an independent statistician who was not involved in the later implementation or statistical analysis.
Blinding
The participants and acupuncturists in our study were not blinded because of the nature of the intervention. Data analysts and outcome assessors were blinded to group assignments.
Interventions
Manual acupuncture was performed with sterile disposable needles (Hwato Needles, Sino-foreign Joint Venture Suzhou Hwato Medical Instruments, China, size 0.25mm*40mm). The needles were inserted into a depth of 15 to 30mm at the acupuncture points and were stimulated manually (lifting and thrusting combined with twirling and rotating) for at least 10s to achieve “Deqi” (a compositional sensation of soreness, numbness, distention, and heaviness). The needles were manually stimulated every 10 min and were retained for 30 min. Participants received acupuncture therapy 6 times per week (Monday to Saturday) for 4 weeks.
Participants were allowed to use Ibuprofen sustained-release capsules (0.3g/T, Tianjin Smith Kline & French Laboratories Ltd., Tianjin, China) as a rescue medication, and the dose should not exceed 1200mg per day. The details of usage were recorded in the case report form (CRF).
Control Group (Local Point)
The selection of acupuncture points in Control Group was based on traditional Chinese medicine meridian theory of Bi syndrome. Nine selected points were ST34 (Liangqiu), ST36 (Zusanli) EX-LE5 (Neixiyan), ST35 (Dubi), SP9 (Yinlingquan) SP10 (Xuehai), GB34 (Yanglingquan), BL40 (Weizhong) and Ahshi point. If one knee was affected, nine points were selected on the affected side, and bilateral nine points were selected if both knees were affected.
Treatment Group a (LI11)
The acupuncture point in Group B was LI11 (Quchi), based on the Yellow Emperor’s Classic of Internal Medicine, contralateral LI11 was selected based on the affected knee, for example, if left knee was affected, the right LI11 was selected, but if two knees were affected, bilateral LI11 was selected.
Treatment Group B (Local Point & LI11)
The acupuncture points in Treatment Group B were the combination of the acupuncture points in Control Group and Treatment Group A (Figure 1).
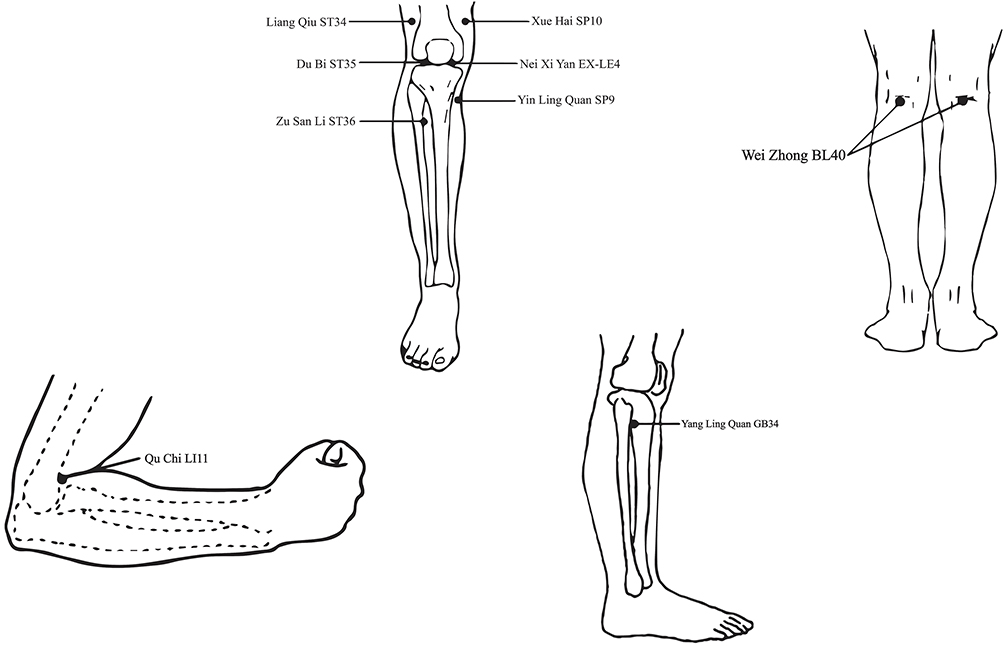
Figure 1 Selected acupuncture points used in the study.
Outcomes
Primary Outcome Measurement
Participants used Visual Analogue Scale (VAS) to evaluate the average pain intensity and McMaster Universities Osteoarthritis Index (WOMAC) function subscale to assess daily ability. The primary outcome was response rate14 which is defined as the proportion of participants whose average VAS scores decrease ≥2 points and the WOMAC function subscale scores decrease ≥6 points at Week 4 compared with baseline. If one knee was affected, the assessment was based on that knee, if both knees were affected, the assessment was based on the worse one (Figure 2).
Figure 2 Schedule for data collection of this trial. Treatment Group: A LI11, Treatment Group: A LI11 & local points, Control Group: local points.
Abbreviations: VAS: Visual Analogue Scale, WOMAC: Western Ontario and McMaster Universities Osteoarthritis Index.
Secondary Outcome Measurement
The secondary outcomes were VAS and WOMAC. VAS is an 11-point self-administrated tool, ranging from 0 (no pain at all) to 10 (worst pain)15 to evaluate the average pain intensity. WOMAC is a self-administered questionnaire consisting of 3 subscales with a total of 24 items. Pain subscale evaluates the intensity of pain in 5 different conditions, stiffness subscale evaluates the stiffness of the affected knee, and function subscale evaluates the ability to move and daily activities. The total score of WOMAC is 68, higher scores indicate worse pain, stiffness, and function16 (Figure 2).
Compliance assessment was assessed at Week 4, participants with scores lower than 80 were considered as poor compliance.
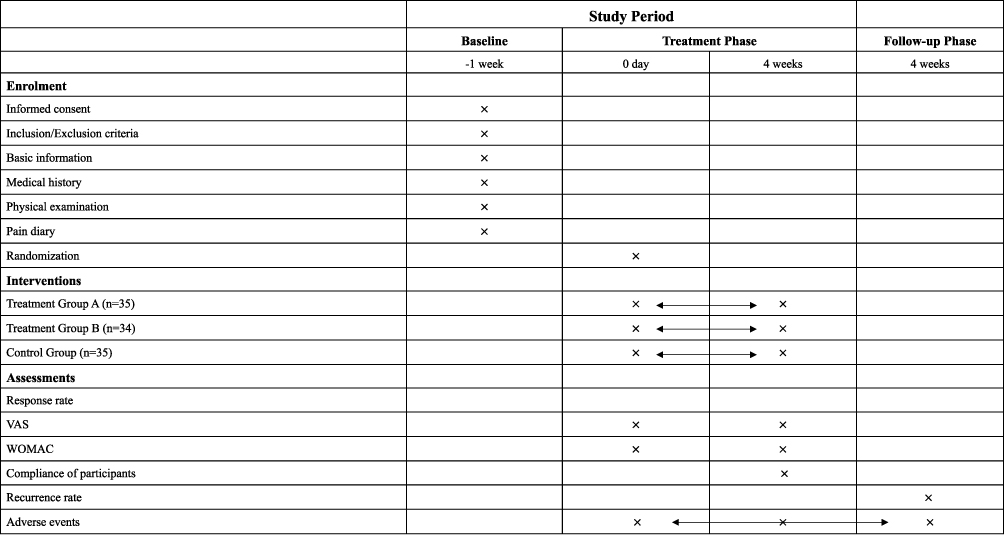
The recurrence rate at follow-up phase was defined as VAS scores increased ≥2 points and WOMAC function scores increased ≥6 points (Figure 2).
Adverse Events
Adverse Events (AEs) were evaluated and recorded by researchers after the end of weekly treatment and during the follow-up phase. Serious adverse events were reported and handled based on regulations. Common acupuncture-related adverse events include dizziness, subcutaneous hematoma, infection, etc.
Sample Size Calculations
No effective response rate of manual acupuncture on LI11 was found in previous studies, while we found one study indicated that a reasonable minimum number of participants from the population of interest is 30.17,18 Thus, a total of 90 participants were needed in our study, considering 15% of dropouts, we decided to recruit 108 participants (36 for each group) to achieve the practical purpose of the trial based on clinical experience.
Statistical Analysis
All data were assessed using R software (4.2.1). Continuous data were described using mean (standard deviation) or median (interquartile range) and the paired t-test (normal distribution) and Wilcoxon rank sum test (abnormal distribution) were used for comparison within groups. Categorical data were described using number and percentage, and the Wilcoxon rank sum test was used for comparison within the group. The chi-squared test was used to compare the response rate, VAS, and WOMAC between 3 groups. α was adjusted using Bonferroni and set at 0.017 for multiple comparisons of response rate and recurrence rate, while α was not adjusted for other outcomes. Adverse events were described using the chi-squared test. All test indicators were analyzed using Intention-To-Treat (ITT), and missing data were obtained using the last observation carried forward (LOCF) method.
Results
Participant Characteristics
We screened 150 participants in total, of them, 42 participants were excluded after screening. A total of 108 participants (36 in each group) were randomized, and 4 participants did not receive allocated intervention due to the pandemic, which was eliminated from analysis, thus 35 participants in Treatment Group A, 34 participants in Treatment Group B, and 35 participants in Control Group were included in the ITT analysis and safety analysis. Among these, 34 participants in Treatment Group A, 31 participants in Treatment Group B, and 28 participants in Control Group completed all treatment at Week 4 (Figure 3).
Figure 3 Trial flow chart. Treatment Group: A LI11, Treatment Group: A LI11 & local points, Control Group: local points.
There was no significant difference in demographic, clinical characteristics or outcome measurements at baseline. The mean (SD) of age and BMI was 60 (5.73) years and 26.35 (3.65) kg/m2. Eighty-four (80.77%) participants were female in our study, and mean (SD) duration of KOA was 5.5 (5.96) years. Almost half of participants (49[47.12%]) were at Grade II of Kellgren-Lawrence grade. The mean (SD) of VAS and WOMAC was 5.48 (1.52) and 34.96 (14.34), respectively (Table 1).
Table 1 Characteristics of the Patients at Baseline
Primary Outcome
In our study, the response rate in Treatment Group A, Treatment Group B, and Control Group was 71.43%, 85.29%, and 51.53%, respectively, at Week 4. The pairwise comparison showed that the response rate of Treatment Group B was significantly higher than that of Control Group (difference[98.3% CI]: 33.86[0.135,0.543], P = 0.003). While there was no significant difference between Treatment Group A and Control Group (difference[98.3% CI]: 20.00 [−0.072, 0.472], P = 0.086), Treatment Group A had a better response rate. Although Treatment Group B had a better response rate compared with Treatment A, no significant difference was found (difference[98.3% CI]: −13.86 [−0.372, 0.094], P = 0.163) (Table 2).
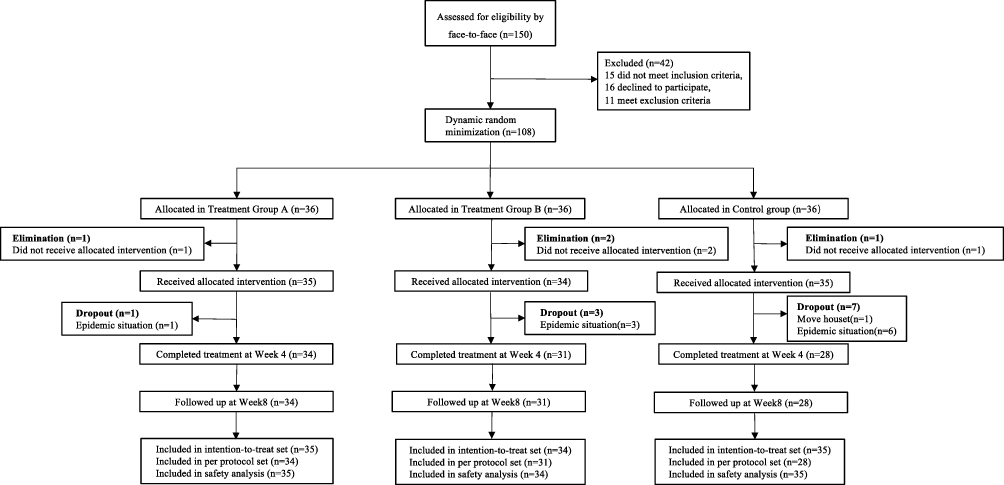
Table 2 Primary and Secondary Outcomes (ITT)
Secondary Outcomes
For VAS and WOMAC, there were significant differences within 3 groups at Week 4 compared with baseline. There was a significant improvement in VAS scores at Week 4 in Treatment Group B compared with Control Group (difference[95% CI]: −1.65 [1.000 to 2.000], P = 0.001) and Treatment Group A (difference[95% CI]: 1.08 [0.000 to 2.000], P = 0.006). Moreover, a statistically significant difference was found in Treatment Group A (difference[95% CI]: 4.39 [1.000 to 6.000], P = 0.006) and Control Group (difference[95% CI]: −7.07 [3.000 to 10.000], P = 0.000) compared with Treatment Group B for WOMAC function subscale at Week 4, and similar results were found in WOMAC pain subscale, and Treatment Group B had significantly better pain relief compared with Treatment Group A (difference[95% CI]: 1.08 [0.000 to 2.000], P = 0.012) and Control Group (difference[95% CI]: −1.65 [1.000 to 2.000], P = 0.001). However, merely Treatment Group B vs Control Group (difference[95% CI]: −0.64 [0.000 to 1.000], P = 0.012) had statistical significance in WOMAC stiffness subscale (Table 2).
The compliance of participants in each group was ≥80%, which was considered good compliance (Table 3). The number of participants who used rescue medication (Ibuprofen) was 6, 5, and 5 in Treatment Group A, Treatment Group B, and Control Group, respectively (Table 3). The recurrence rate was highest in Control Group (34.29%), and there was no significant difference in pairwise comparison. We also performed sensitivity analysis using Per-Protocol analysis (PP analysis), the results were similar with ITT analysis (Table 4).
Table 3 Compliance Data, safety Assessment and Rescue Medication Usage
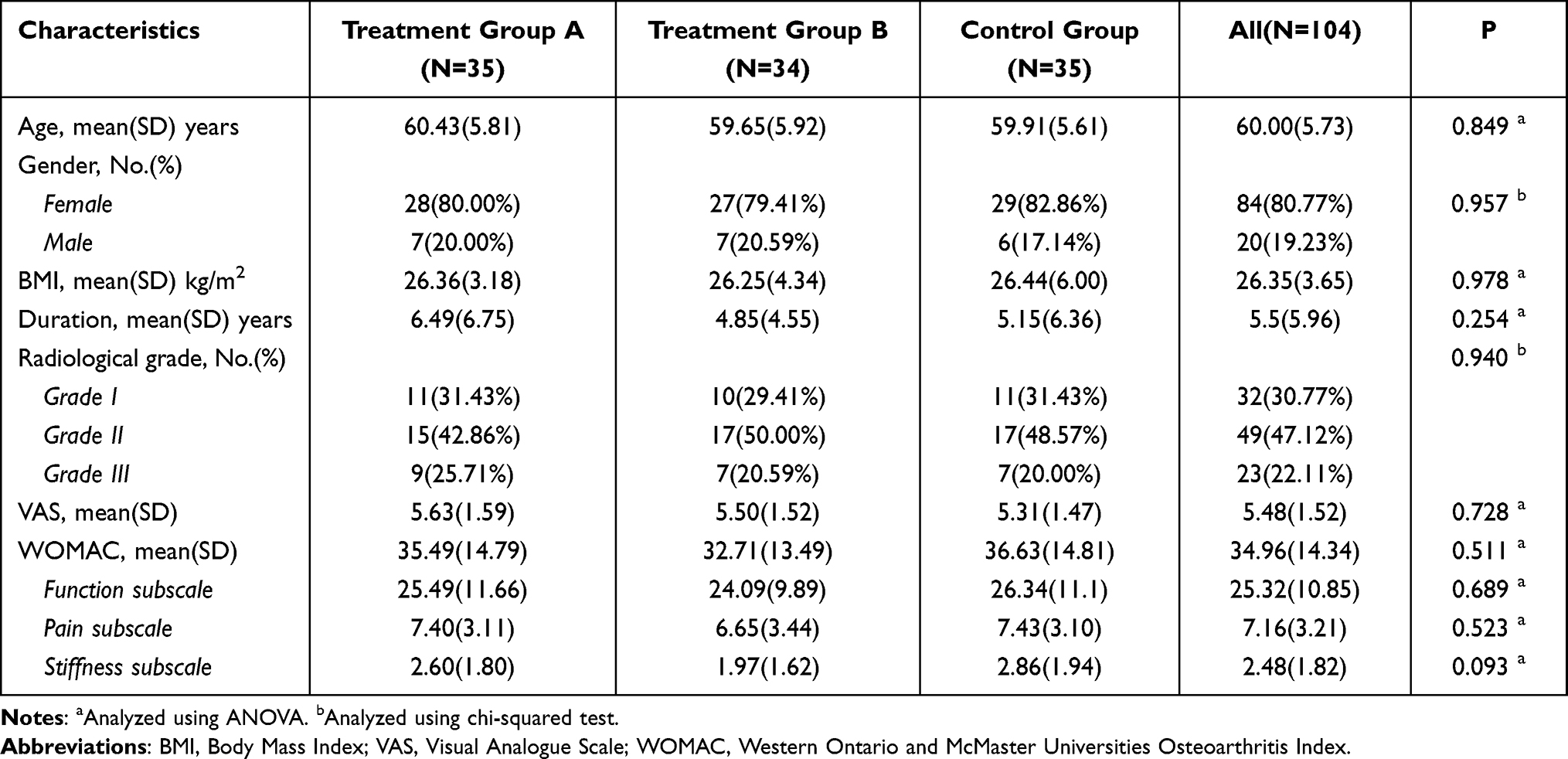
Table 4 Primary and Secondary Outcomes (PP)
Safety
No severe adverse events were found among all three groups. A total of 8 adverse events (8/104) occurred in our study (Table 3), 4 participants had subcutaneous hematoma, and 4 had subcutaneous hemorrhage, all participants healed completely within one week. There was no significant difference among three groups.
Discussion
In our study, participants with KOA who received acupuncture at LI11 had a better response rate than those who received acupuncture at local points. Meanwhile, participants improved better regarding pain and dysfunction in LI11 group compared with local point group. Besides, the combination of two selected points showed best in alleviating pain and dysfunction. No severe adverse events were found among all three groups, and participants who had adverse events such as bleeding healed completely within one week. These results indicated that LI11 may be an effective point for patients with KOA, and it could be used as a selection for young acupuncturists and acupuncturists who work in rural areas; however, large-sample studies are required to further verify the results in the future.
To our best, there is no study comparing LI11 with local points for patients with KOA. However, we found two studies comparing distal points with local points for chronic pain, and they have consistent results with ours. Irnich et al19 found that acupuncture at distal points had better effects in improving flexibility and pain for patients with chronic neck pain compared with dry needling at local myofascial trigger points. Also, Yu et al11 found better pain relief and knee range of motion improvement after acupuncture at distal points than local points in treating KOA. The underlying mechanism of acupuncture at distal points in reducing pain might be related to non-segmental antinociceptive systems, whereas there is limited evidence to demonstrate non-segmental antinociceptive systems, thus more studies need to be done to investigate the mechanisms.
Our study has several limitations. First, we merely used two self-administered outcome measurements to assess the pain and function of patients with KOA. KOA affects the quality of life and mental health as well, thus questionnaires such as SF-36 are necessary. However, the main goal of KOA treatment is to relieve pain and dysfunction, VAS is the most common tool for evaluating pain, and WOMAC is the most common tool for KOA assessment. Secondly, we did not use sham control which is not always the best control in different studies. Our study aimed to detect the effectiveness of acupuncture at LI11 compared with acupuncture at local points which has been proven effective. Moreover, the positive control was more ethical for participants who were seeking relief from their discomfort. Thirdly, the participants and acupuncturists were not blinded in our study, thus it is difficult to exclude the placebo effects. Finally, the sample size in our study was relatively small, thus it is hard to generalize our results. However, this is a pilot study which could provide hints for future studies.
Conclusion
Based on our current results, compared with acupuncture at local points, acupuncture at LI11 had better effects in alleviating pain and dysfunction, indicating that acupuncture at LI11 could be a choice for young acupuncturists and acupuncturists who work in rural areas; however, large-sample studies are necessary to further verify results in the future.


